Introduction:
Each year 7,400 women are diagnosed with ovarian cancer in the UK. When diagnosed early, the prognosis for this type of cancer is good, however it is often already in its advanced stages by the time it is diagnosed. This is because it is more common in elderly people who no longer tend to attend regular gynaecological examinations. Since these tumours are not usually symptomatic until they are in the advanced stages, diagnosis is often made when the disease has advanced or spread and is more difficult to treat. There is often no specific or effective treatment for these patients. Therefore, we urgently need specific and effective therapies to treat advanced ovarian cancer.
Description of the Project:
One of the most promising avenues of research in the quest for new ovarian cancer treatments is the manipulation of the immune system, namely Immunotherapy. The project’s current focus is on various aspects of this type of therapy. Several projects are currently being developed that focus on the immune system as a gateway to better therapies, for example:
- Developing antibody-drug conjugates against ovarian tumour cells
- Working on predicting which ovarian cancer patients will respond best to current immunotherapy treatments
- Investigating how to increase the effectiveness of T-lymphocyte-based immune cell therapies in ovarian cancer patients (this work is largely being carried out at the CRIS Unit for New Experimental Therapies)
Antibody-drug conjugates:
It is often difficult to find effective targeted treatments for ovarian cancer cells that do not harm other healthy cells. Antibodies, which function as biological guided missiles, can be used resolve this. If we identify a molecule that appears mainly on the surface of tumour cells and not in healthy cells, we will be able to direct antibodies against that molecule. If we also couple a chemotherapy drug to that antibody, we can direct the chemotherapy on the ovarian cancer cells. This approach has already been successful for Dr Pandiella and Dr Ocaña in breast cancer.
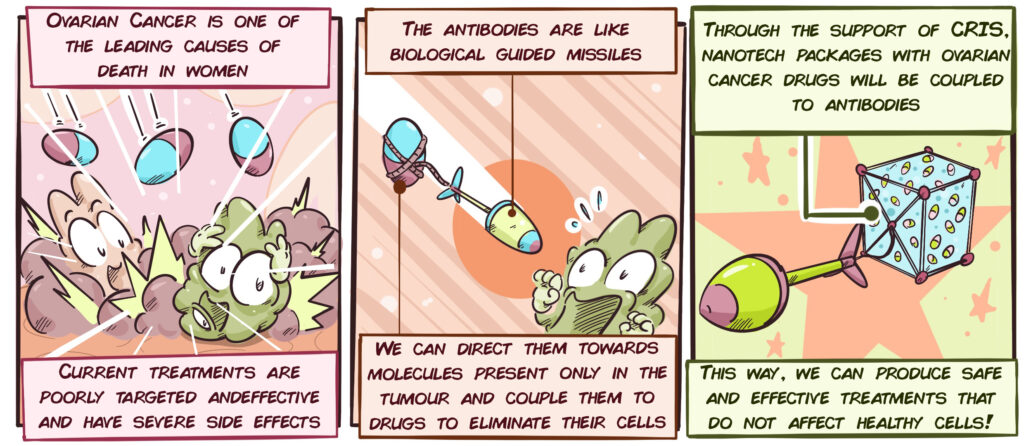
Until now, most antibody-drug conjugates have been created by binding antibodies to chemotherapy drugs, however these drugs do not target the characteristic weak points of ovarian cancer cells. This is because many of the more targeted therapies lose some of their function by being bound to antibodies. To resolve this, Dr Ocaña’s team is working with nanoparticles, which act like little nanotech “packages” that contain these targeted therapies without changing them. If we couple these “packages” to the antibodies, we will have access to therapies directed at ovarian cancer cells that also attack specific ovarian cancer weaknesses for the first time.
Identifying patients that will respond to Immunotherapy:
In many solid tumours, such as those of the ovary, tumour cells are capable of switching off and paralyzing T lymphocytes. We could consider these tumour cells our cellular warriors tasked with destroying the T lymphocytes. Certain immunotherapy treatments, known as immune checkpoint inhibitors, reawaken these lymphocytes so that they re-attack the malignant cells.
This approach offers a source of hope for patients with advanced ovarian cancer as it has had excellent results in other advanced cancers. However, immunotherapy still does not work for all patients. It is essential to be able to predict which patients will benefit from these treatments in order to identify them before treating them and to avoid using the treatment on patients who will evidently not respond appropriately. The aim of this part of the project is to attempt to find ways to predict the response to immunotherapy in ovarian cancer patients.
Latest developments:
The various approaches to research on Immunotherapy in Ovarian Cancer continue to progress swiftly, despite the difficulties presented by the pandemic.
For some time, our researchers have been working to develop antibody-drug conjugates to fight ovarian tumour cells. This system has already been developed with considerable success in the CRIS Breast Cancer Project. As we said previously, antibodies are like guided missiles that detect and bind to a specific molecule. Using state-of-the-art techniques, researchers are identifying elements on the surface of ovarian tumour cells that are not present in other cells and enabling them to be differentiated. It is a complex and detailed process, which involves many stages as we are having to look for molecules that are only on the surface of the tumours and that do not appear in healthy cells. At all costs, we must avoid the antibodies accidentally binding to the healthy cells and damaging them.
To date, 12 proteins that are only present in ovarian tumour cells and not in healthy cells have been identified. Work on developing antibodies against these proteins is currently underway to find out which are most effective against ovarian cancer.
With regard to identifying and predicting which patients will respond best to immunotherapy, researchers recently published an article in the Frontiers in Oncology journal (more information here) on other immunotherapy treatments for ovarian cancer.
Following an exhaustive analysis, the team has discovered that when there are elevated levels of certain combinations of molecules in the tumours of ovarian patients and signals from the immune system, this correlates with greater immune system activity in the tumour and a greater response to immunotherapy. Although further studies are needed, this work offers a vital key to detecting which patients may benefit most from immunotherapy.
Another of the group’s recent findings is a new possible weak point in ovarian cancer cells. This is a protein involved in several key tumour cell processes, called ERK5. The group is currently studying the molecular mechanisms that help determine whether this molecule is a good target for treatments. The team hopes to publish the results of this research shortly and start developing compounds against this protein. This is due to the fact that, at present, there is no available drug that targets this protein.