Introduction:
Cancer immunotherapy has brought about a radical change in the way in which many types of cancer are treated. However, although has fantastic results in some patients, in a significant percentage such therapies are ineffective. Knowing which patients have a greater or lesser chance of responding is one of the biggest challenges of modern medicine: it is essential for this probability of response to be determined in order to identify and treat only those patients who will benefit from immunotherapy, opting for alternative approaches for the remaining patients. To date, most attempts to predict how a patient will respond to immunotherapy have focused on tests that rely heavily on patient biopsies. However, Dr Raquel Pérez-López’s group, is researching different, less invasive methods such as diagnostic imaging techniques.
The project:
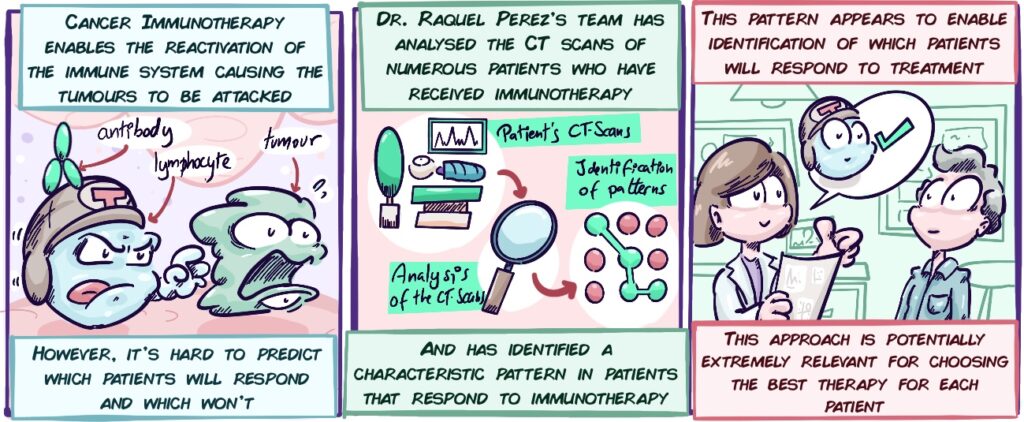
Computational analysis of the medical images (MRIs, CT scans, etc.) enables each patient’s tumour to be understood in greater detail and, therefore, for the characteristics of the tumours that make them more responsive to immunotherapy to be identified. Two types of research are combined in this ambitious research project: analysis of these medical imaging data using computational techniques and an in-depth study of the tumour genes. Through studies such as these, we are increasingly progressing towards precision medicine.
Objectives:
The project analyses routine patient imaging techniques (such as tomography or CT) and other more complex techniques, which provide information on the functioning of tissues (such as diffusion and perfusion Magnetic Resonance Imaging). This will be combined with genetic testing of the tumour cells. Integration of all these data will enable more reliable information to be obtained on which patients will respond (and are responding) to immunotherapy. The objectives of this study include:
- The VHIO Radiomics group produced a “fingerprint” (or signature) from radiological images (X-rays, CT scans, etc.). This signature may be able to predict the response to immunotherapy. One of the objectives of the project is to verify that this is the case.
- Creation of a magnetic resonance imaging (MRI) signature that enables the response to immunotherapy to be predicted.
- Creation of a model that integrates the image data (CT, MRI) with data from the genetic studies of the tumour cells and patient information and can predict the patient’s response.
- Identify changes in the first few weeks of immunotherapy to enable prompt determination of whether or not patients are resistant to immunotherapy.
- Develop an application to be used in clinical practice that implements the models and patterns developed by the group.
Results update:
Despite complications arising from the COVID-19 pandemic, Dr Raquel Pérez’s group has reached some significant milestones in the project’s development. The objectives of the project include computational analysis of the patients’ CT test results and the identification of a pattern, or signature, which recognises which patients respond to immunotherapy and which who do not.
Some of the group’s results were recently published in the international journal Radiology, one of the most prominent in its field, in an article entitled “A CT-based radiomics signature is associated with response to immune checkpoint inhibitors in advanced solid tumors”. The group’s results demonstrate the success of its CT signature in predicting which patients are more likely to respond to immunotherapy. Although the efficacy of this signature is yet to be developed further, these results confirm that Dr Raquel Pérez’s group’s approach is extremely promising and could significantly help to decide which patients to treat with immunotherapy.