Context
Tumours of the central nervous system are the second most common form of childhood tumour, after acute leukaemia. However, they are still the leading cause of death in childhood cancer on account of their heterogeneity and the difficulty in treating them effectively.
One of the most aggressive types of brain tumour in children is the Diffuse Intrinsic Pontine Glioma (DIPG). They are the most common brainstem tumours in children, representing approximately 75-80% of all paediatric brainstem tumours. It almost exclusively affects children aged 4 to 11, and there is currently no cure. Children who develop such a tumour have a very short life expectancy and most die within 18 months of diagnosis.
One of the biggest problems is that they develop in the pons (middle) of the brain stem, an area of the brain responsible for essential life functions. This area of the brain regulates breathing, eye movement and even the heartbeat. Therefore, surgical intervention in this area is too dangerous and cannot be performed.
Another characteristic of DIPG is that they tend to produce metastasis in other areas of the brain, which makes it difficult to control the disease and often causes treatments to fail. In fact, the cells move and spread so rapidly that in many cases treatment is not able to kill tumour cells at the rate at which they are spreading.
As this type of cancer is only found in children and is relatively uncommon, it is difficult to conduct clinical trials owing to a lack of patient numbers. Furthermore, molecular studies show that these kinds of tumours are very different from adult gliomas, and so they cannot be treated in the same way as adult tumours. In fact, childhood DIPG cells spread 10 times faster than gliomas in adult patients.
It is, therefore, essential to identify genes and mutations capable of explaining this ability to migrate and invade, in order to identify weaknesses in these cells and develop more effective treatments against metastasis.
Project
The project, launched at the end of 2019, aims to identify alterations in tumour cells that would allow us to predict which children are more likely to develop metastasis. If we are able to discover which genes in tumours can cause metastasis when they are altered, we will be able to identify children who are at greater risk and provide preventative treatment.
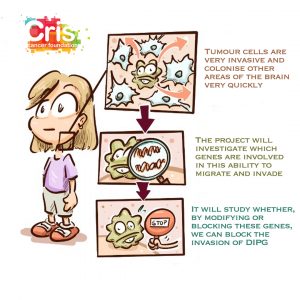
The first part of the project, therefore, is based on identifying genes that, when altered, may trigger increased migration and invasion. At present, 10 candidate genes have been found, two of which will be selected for validation in the next part of the project.
Once the team has identified which mutations trigger metastasis, the second objective is to verify whether compounds which can stop these alterations can prevent metastasis in experimental models.
For this purpose, animal models will be used, incorporating DIPG cells and attempting to block their ability to metastasise. These models provide an enormous amount of information, but faster and cheaper models are also required, which can be more easily manipulated. Given that experiments on cultivated tumour cells do not emulate the complexity of brain tissue, the project team has sought an ingenious alternative to perform experiments: keeping slices of animal brain cultivated in petri dishes in order to conduct experiments on them. These models offer a huge advantage, since they include many types of cells, including healthy cells, tumour cells and even neurons, maintaining the architecture of tissues, interactions and communication. This is a very advanced type of experiment that very few groups are able to perform.
If these models yield positive results, they can be very quickly applied in clinical practice, as the results can be translated into new, more effective treatments to halt metastasis.