Principal Investigator: Dr. Alan Melcher, Prof. Kevin Harrington
Introduction:
Head and neck cancer is a very common type of tumour (550,000 cases a year worldwide and 12,238 in the UK). Despite being common, mortality rates are still high (380,000 deaths a year worldwide and more than 4,000 in the UK). Most of these deaths occur when the disease spreads or recurs, something that happens fairly frequently, unfortunately. However, even when the tumour is eradicated completely, this type of disease can leave behind some major physical side effects.
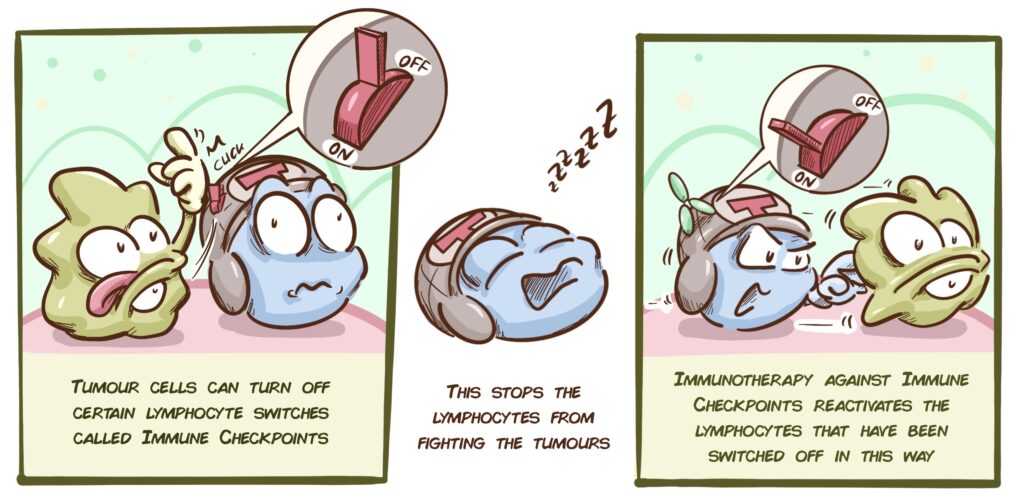
Immunotherapy has had an enormous impact on head and neck cancer and has opened the way for a huge range of possibilities.
- In patients with a single localised tumour (one which has not metastasised), it may be combined with other treatments to jointly achieve a less aggressive therapy for patients with fewer side effects.
- In patients with tumours that have spread or recurred, it may result in therapies with better outlooks than currently available options.
Nevertheless, the truth is that immunotherapy only works in some patients at this time and, unfortunately, there are presently no effective methods for predicting which patients will respond to treatments using immunotherapy.
One of the biggest problems when it comes to designing new and better immunotherapy treatments is that both the tumour and the immune cells that fight against the tumour change over time, partly due to the treatments given. Being able to understand these changes would allow us to design better immunotherapy strategies and even predict which patients are likely to have a better response to such treatments.
With this challenge in mind, and with CRIS’ assistance, the Centre for Translational Immunotherapy (ICR) has been created.
The structure:
This project will be directed primarily by the Targeted Therapy Team, led by Dr Kevin Harrington, who has been working on the development of new therapies against one of the hardest-to-treat tumours, i.e. head and neck, since 2001.
The other pillar of the project is the Translational Immunotherapy Team, led by Dr Alan Melcher, who has vast experience in the treatment of solid tumours using immunotherapy.
The project:
Our immune system is ready to fight against any type of threat, including cancer, and the T-cells are key elements in this process. We have millions of different T-cells in our body, each one with its own receptor that allows it to identify and destroy a different threat. Whenever a threat, such as a tumour cell, appears, the T-cells with receptors which recognise that specific cell are triggered and destroy it. However, tumours sometimes manage to evade or trick our immune system and that is when they begin to advance.
In order to understand our immune response better and determine the best way to trigger a response using immunotherapy, this project will study how this immune response changes over time in patients with head and neck tumours. A large number of samples taken from patients who have received different types of treatments will be used to analyse:
- Which T-cells are present at each stage of the tumour’s development, before and after the various treatments. T-cells are characterised by examining which receptor is present in each T-cell in the tumour. This will allow us to accurately determine which aspects of the tumour they are fighting against;
- The activity of other elements of our immune response. Our immune system has a tremendous number of components and these can trigger a variety of mechanisms based on the type of threat it is facing. It is therefore essential to determine which elements are present during the different stages of each patient’s disease.
This will be achieved using the latest and most advanced genetic and molecular analysis methods. Improving our understanding of a person’s immune response will shed light on what is happening in each patient over the course of their disease; play a huge role in helping us to identify which patients have the best chance of responding well to immunotherapy; and allow us to develop better immunological treatments.