Background:
Mesothelioma is a type of thoracic tumour that occurs in the mesothelium. This is the cell layer that covers several of the organs contained in the thoracic cavity. We now know that one of its main causes is exposure to asbestos (also called amianthus). Although asbestos now appears to be a thing of the past, a large number of people of middle-advanced age have been exposed to these minerals over extended periods during their lifetimes. Furthermore, the asbestos industry has a large presence in developing nations, which means that large groups of people may be exposed to these extremely dangerous materials. Therefore, mesothelioma is an increasingly significant public health concern.
Using ambitious and highly innovative approaches, Dr Klampatsa has spent many years developing new immunotherapy-based treatments to combat these types of tumour.
The Project:
Dr Klampatsa’s group focuses on two primary approaches.
CAR T-cells to combat thoracic tumours:
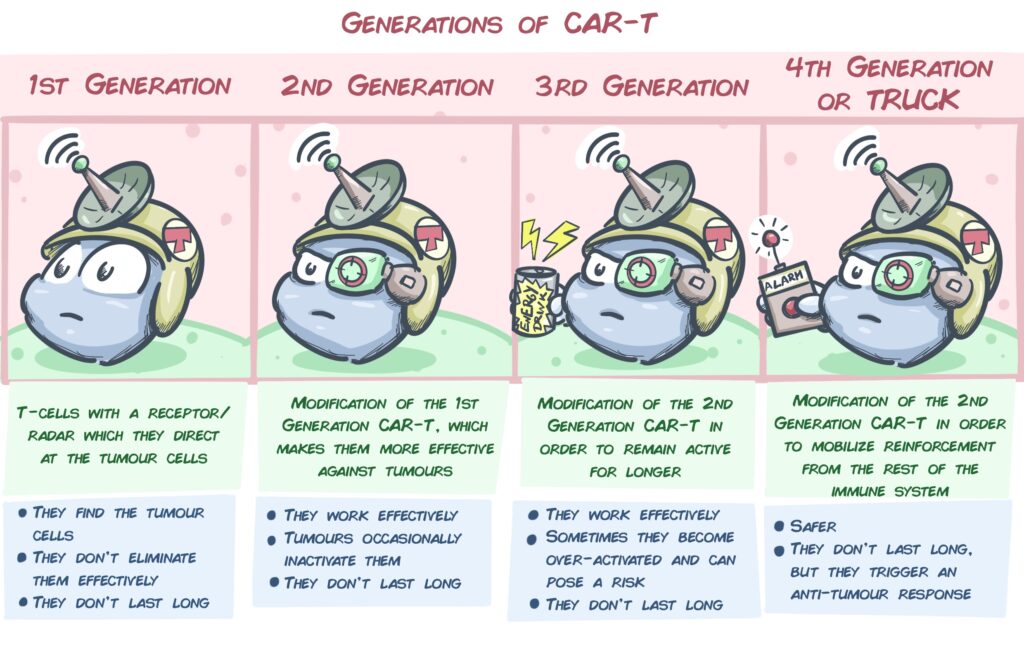
CAR T-cells consist of T-cells (a type of immune system cell that efficiently kills malignant cells) that have been genetically engineered to include a radar-like receptor. This receptor targets certain molecules that we know are only present in tumour cells. In this way, the T-cells detect and destroy the tumour. Over the years, several generations of these CAR T-cells have been developed, and their results on blood tumours have been very promising.
However, in solid tumours, such as mesothelioma, it appears that the tumour’s surroundings (the tumour microenvironment) are capable of progressively inactivating the CAR T-cells and limiting their efficacy.
In addition to the tumour-detecting receptor/radar, 4th generation CAR Ts (or TRUCKs) regularly emit alarm signals that attract other cells as reinforcement, as substances that modify the tumour microenvironment and prevent the CAR’s activity from being blocked. In short, in addition to their own anti-tumour activity, they contribute to the development of an effective immune response against the tumour. Dr Klampatsa’s group is focusing on this type of CAR T, or TRUCKs. The group’s objective is to develop TRUCKs directed at mesothelioma cells and that, concurrently, alter the microenvironment. This will lead to a greater rejection of tumour cells. Once they have been developed and approved, they will be put into practice in clinical trials.
Immune Checkpoint Immunotherapy:
The second approach focuses on another type of immunotherapy, which involves molecular T-cell switches called Immune Checkpoints. Although T lymphocytes are very efficient against tumour cells, they can sometimes activate these switches and inactivate the T-cells. Fortunately, there are antibody-based immunotherapies that can restore activity to the T-cells.

However, this type of immunotherapy does not work on all patients. It is estimated that only 40-50% of patients treated with it respond to the treatment. It is therefore essential to find ways to identify and select patients that will respond and only administer immunotherapy to these patients.
In order to identify possible biomarkers or elements that enable these patients to be identified, Dr Klampatsa’s group will study samples from a large number of mesothelioma patients from various hospitals in depth. These samples will be obtained at the point of diagnosis and after patients have been treated with immune checkpoint immunotherapy. In this way, it will be possible to see the changes in the tissues, the immune system and the tumour microenvironment in patients who do and do not respond well to treatment. This data will be key to understanding what happens in each group of patients and for developing diagnostic methods that enable the patients that will respond appropriately to Immune Checkpoint treatments to be identified.