Breast cancer is the most common cancer in the UK. Around 55,200 people are diagnosed with breast cancer every year in the UK. That is around 150 people a day.
15 out of 100 (15%) of all newly diagnosed cancers in the UK are breast cancer.
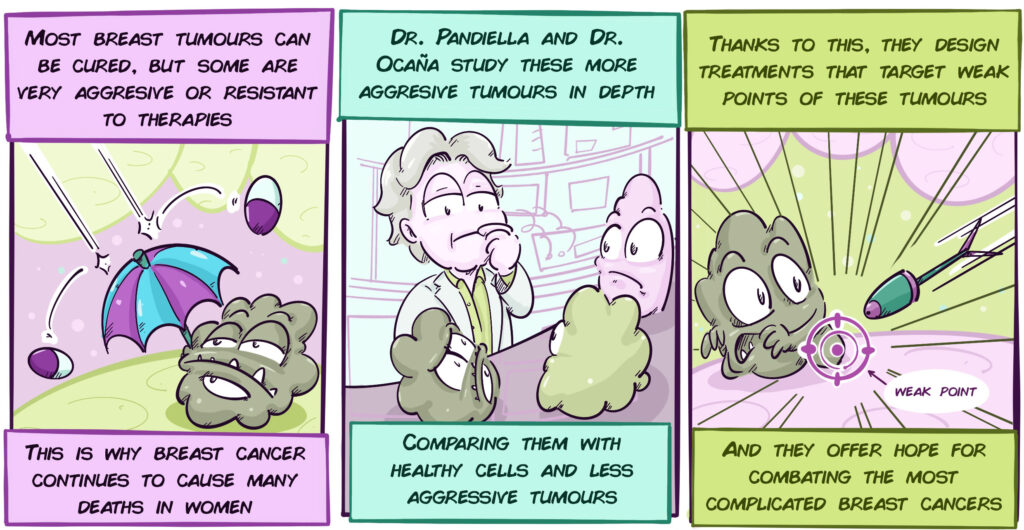
Although the great majority of breast tumours are cured, even today almost 20% of patients do not survive. Resistance to treatments or the absence of specific therapies for some types of breast cancer are the main reasons that certain tumours cannot be completely eliminated.
Doctors Atanasio Pandiella and Alberto Ocaña have been working for years on breast tumours with the worst prognosis or that become resistant to treatment, trying to analyse in molecular detail each type of tumour and search for appropriate therapies.
Much of their efforts are devoted to the two most aggressive subtypes of breast cancer, triple-negative tumours, and HER2+ tumours :
Triple-negative Breast Cancer is called this because the tumour cells lack certain molecules that define other types of breast cancer. These tumours have a very poor prognosis, and there is currently no specific therapy against them. Research in this field is therefore urgently required to develop effective therapies against these types of tumours.
On the other hand, HER2+ breast cancers are very aggressive tumours whose cells have a large amount of a protein called HER2, which is the main cause of their malignant transformation. The lives of these patients changed when, at the end of the 1990s, HER2-targeted therapies were designed to treat these tumours very effectively. However, the current problem of these therapies is that despite their high efficacy, a significant number of patients develop resistance to them over time. Therefore, it is imperative that research provides new ways to treat these patients.
Project Description:
The research on breast cancer in which Atanasio Pandiella and Alberto Ocaña work together can be grouped into three projects. They address new therapeutic alternatives for the most aggressive types of breast cancer:
Triple Negative Breast Tumours Project:
This innovative project involves using the latest molecular and genetic analysis tools to identify elements on the surface of triple-negative tumour cells and distinguish them from healthy cells. Once these characteristic molecules are determined, antibodies will be generated against them, which, like a guided missile, will carry a specific drug against the tumour cell. Another type of study will attempt to make immune system cells capable of recognising tumour cells as foreign and attacking them.
| DRUG |
| ANTIBODY |
| TUMOUR CELL |
| Tumour cell-targeted antibodies coupled to drugs |
HER2+ Breast Tumours Project:
To study how resistance to the usual treatments against Her2+ tumours arises, the researchers of this project are developing several laboratory models that simulate this resistance. For example, they create cell lines that are resistant to various treatments. They then compare, by molecular or genetic methods, these resistant cells with normal cells or tumour cells that are not resistant to treatment. In this way they manage to find unique characteristics of treatment-resistant tumour cells. These characteristics can become weak points against which to design new treatments.
Another similar approach, but with a different take, is to study tumours that respond very well to therapies and look for what characteristics those tumours have. Although technically this approach is complicated, it can provide enormous clues to understand which mechanisms of tumour cells we need to target to achieve better therapies against this aggressive type of cancer.
Latest developments:
HER2+ Breast Tumours:
Researchers from the CRIS Breast Cancer Project, in collaboration with Italy’s G D’Annunzio Chieti-Pescara University, have developed a potential treatment for patients whose tumours have become resistant to anti-HER2 therapies.
The therapy is based on the observation that tumours of patients who have high levels of HER2 also have high levels of a similar protein, HER3. Virtually no other cell in the body has very high levels of HER3, which makes it relatively easy to specifically identify and target these cells. To this end, an antibody was designed (such as those being developed for triple-negative tumours) that attaches highly effectively to HER3. In addition, this antibody has a drug attached to its tail that destroys the skeleton of tumour cells. The antibody binds only to tumour cells with HER3, ignores healthy cells, and eliminates only tumour cells, so this therapy has very few side effects. The good laboratory results have been published in a prestigious scientific journal and have opened the door to further clinical trials (Learn more here).
Another of this group’s advances focuses on new modifications of trastuzumab, one of the first treatments developed against Her2+ tumours. It binds HER2, disables it, and the tumour cell dies. However, as many patients develop resistance to these treatments, work has been underway for years to modify the treatment and prevent resistance. One of these new treatments is a newly approved therapy in the USA called Trastuzumab-Deruxtecan. Dr. Pandiella’s laboratory is studying in laboratory models whether the use of this new therapy helps avoid overcoming HER2+ tumour resistance. This will help to better understand when to use this drug and what additional indications it may have.
Finally, thanks to their ongoing work on identifying why Her2+ tumour patients stop responding to treatments, they have just identified a new mechanism by which tumour cells become resistant to therapies. The results of this work will be known in the coming months.
Triple Negative Breast Tumours Project:
Triple-negative breast cancer, unlike other types of breast cancer, does not have a clear weak point to target with drugs. Although a great deal of work is being done to find specific treatments for this type of cancer, for the time being chemotherapy is still the most widely used option.
Recently, the use of a class of drugs called BET inhibitors has been studied. These drugs prevent tumour cells from triggering some of the mechanisms that allow them to multiply and expand. The problem is that as with many other treatments, tumour cells become resistant to these treatments.
In this group, researchers have seen that tumour cells, when they become resistant to BET inhibitors, become vulnerable to other drugs: Inhibitors of a protein called PLK1. Interestingly, there are PLK1 inhibitors already in clinical trials, such as volasertib, so it opens a door to possible clinical trials using this strategy: use BET inhibitors to treat triple-negative breast cancer and use volasertib to prevent tumour cells from becoming resistant to this therapy.

| BET inhibitors block mechanisms that allow tumour cells to multiply | However, tumour cells can become resistant to these treatments | PLK1 inhibitors (such as volasertib) may therefore be used when tumour cells are resistant to BET inhibitors |
| BET-i | BET-i | PLK1 inhibitor |
| Therefore, they have the potential to treat triple-negative breast cancer, for which there are still no specific therapies | This work shows that when this occurs, tumour cells become sensitive to anti-PLK1 treatments | This strategy can be very promising to treat triple-negative breast cancer |
As for the design of antibodies combined with drugs against triple-negative tumour cells, the project is progressing well. After a thorough analysis of the proteins and genetic material of triple-negative tumour cells, our researchers have identified a good target against which to direct drug-conjugated antibodies (see explanation of the project above). Early analyses, performed on tumour cell models, show that an antibody against this molecule may be effective against triple-negative breast tumour cells. Interestingly, they have also observed that this target is not only found at high levels in these breast cancer cells but may also be elevated in colon cancer. They have conducted a series of preliminary studies that show that drug-conjugated antibodies could be very useful in this type of cancer. Such surprises are frequent in the study of cancer and highlight the importance of research: the study of the molecular details of one type of tumour cell can provide very important clues about other cancers or even other pathologies. In fact, the findings in HER2-positive tumours in breast cancer also led to the application of HER2-targeted therapies for HER2-rich gastric tumours.